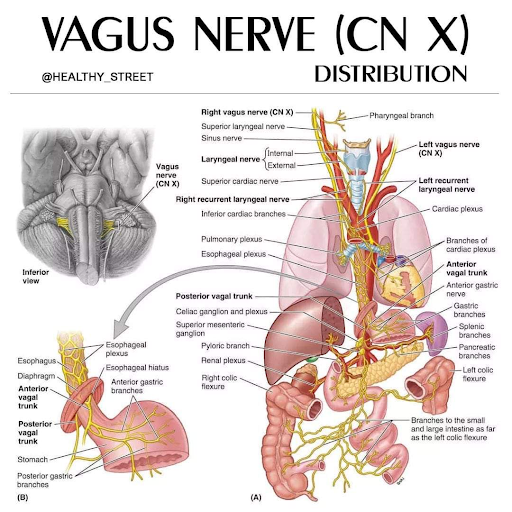
Have you caught the buzz around the vagus nerve? There is a lot of information about it – and rightly so, it is one of the most complex nerves in its function as well as its trajectory. That’s because it wanders (in latin the word is ‘vagus’) throughout the trunk and abdomen, touching on every organ in some way. If you have had any consistent treatment with our practitioners, this is why we always emphasize how to breathe. This is certainly something that has been a struggle in our post Covid patients with long hauler syndrome. Their system appears stuck in sympathetic activity: difficulty getting a full breath, and elevated heart rate – paired on top of the aftermath of inflammation of getting the virus – fatigue, brain fog. Some have even developed worsening GI symptoms, and bladder dysfunction. All the covid patients we have seen – even some post vaccine – the body guides us towards a restriction surrounding the trajectory of the vagus.
What does the body perceive as stress?
We have learned earlier this year on our blog a bit about how the vagus nerve gets pushed out of commission in response to an external trauma stressor resulting in behavioral symptoms of fight, flight, freeze, fawn (a sympathetic state)(Trauma is a catch 22 state because it can put the vagus nerve out of commission … but its needed to return to homeostasis. That won’t be the emphasis of this article. We’re one step down from trauma = stress).
Inflammation and pathogen fighting is a stress to both the immune and nervous system. It’s internal, but it sets off alarm systems the same way our eyes or our thought patterns might from what they perceive of an external threat. The ability to bounce back immunologically from that infection depends, in part, on the vagal nerve tone (which objectively can be measured by HRV, heart rate variability). Since the vagus nerve has more capacity to report from the body to the brain, all the choices and exposures – up to the point of overload – influence how well it will work to “bounce back.” How you physically posture and emotionally express yourself, how/what you breathe, how/what you digest, literally provides a feedback loop for what and how your body should respond – either to stay in stress (sympathetic fight or flight), or moving into relaxed expansion (parasympathetic, rest and digest). Stress frequency and VARIETY is important for life and growth, and depending on how one responds (or learned to respond) to that stress influences the vagal nerve tone. The vagus nerve plays a primary role in returning the body away from whatever “modes” were stressed from the event (emotional, hormonal, neurological, digestive, immunological) back to non-stress/recovery/slower pace (parasympathetic), and it does better in an acute situation when its had practice and time beforehand to regulate that shift.
What does the vagus nerve have to do with inflammation as it relates to an acute infection, and our ability to fight it off? Does our nervous system really tell the immune system what to do?
Lets learn about how the vagus nerve can also be utilized to keep balance as the immune system fights an infection, as well as turning the tide of recovery. Because yes, two different body systems with different functions and roles actually do communicate with (dare I say, value) each other.
Turns out there are several realities called neuroinflammatory reflexes. One of them is through the splenic nerve (nerve to the spleen). T cells (a type of adaptive white blood cell) in the spleen filter out foreign pathogens. When the vagus nerve is firing well and freely, its function acts on neural plexi, called ganglia. The celiac ganglia once its heard from the vagus nerve, communicates to the spleen via a different neurotransmitter which, when the T cells (a type of white blood cell) picks up on this neurotransmitter (because it has this specific neurotransmitter receptor), it performs a slightly different action, resulting in the production of less pro- inflammatory mediators and chemicals from T cells. Less pro inflammatory signals means a shift towards more signals that are RESOLVING of inflammation (which, is also a role the immune system SHOULD play – clean up the mess of fighting infection. Where there are cytokine storms, or chronic pain that doesn’t got away, the immune system is not getting the signal it should be to clean up the mess). This communication pathway and outcome in the spleen also works to keep antibodies (which are a B cell mechanism) under control – which is important to prevent autoimmunity.
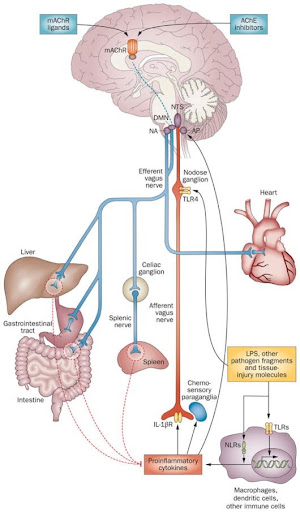
This mechanism works via a specific neurotransmitter, acetylcholine. The receptors for acetylcholine are also in other cells of the body – namely white blood cells, but also in immune cells specific to the liver, and within the smooth muscle of the gut. This is a summary of just a couple articles and one aspect of the immune system through neurotransmitter receptors that are present on white blood cells. So, in short, YES, your nervous system, specifically via the vagus nerve, DOES influence how your immune system does what it does.
Sources: https://pubmed.ncbi.nlm.nih.gov/22665702/ https://pubmed.ncbi.nlm.nih.gov/26512000/
How do you know if your vagus nerve has good “tone” aka, is operating in the way we want it to maintain homeostasis?
The best objective way we have to measure vagal nerve tone/health is called Heart Rate Variability. This is something that has to be calculated after recording heart rate changes with deep breaths over a few minutes. An app like HeartMath or a heart rate monitor is the best way to know for sure. A higher HRV means better vagal nerve function.
Non objectively, aka subjectively, we can surmise that might be the case based on symptoms/diagnoses. And this is kindof determined backwards from what studies have been done on symptoms/conditions that have responded well to transcutaneous vagal nerve stimulation (tVNS), which I’ve listed below. So, if those symptoms or history is present, then one could surmise that their vagus nerve needs some more help.
Vagal nerve stimulation is a fairly recent modality that has gotten attention in the past year, in part from its use on Covid patients who were progressing into severe stage needing ventilation due to cytokine storms. A transcutaneous neural stimulation (or TENS unit – a device used through electrical pads on the skin for nerve symptoms) applied with a special clip to the auricular branch (of the ear) of the vagus nerve has been shown to improve vagal tone/HRV (https://pubmed.ncbi.nlm.nih.gov/25164906/).
Specifically to Covid, transcutaneous vagal nerve stimulation (tVNS) has been used in 2 case studies last year as intervention for 2 patients with worsening Covid (the stage before needing intense ventilatory support). This was looked at specifically in treatment of cytokine storms characteristic of stage 3 progression. Use occurred after a week of infection with worsening progression. When applied via a special clip to the ear for 60 min/day on day 8 of sickness, with no changes in medications. 3 days later O2 saturation improved. A week later, after continued use, his symptoms and objective inflammation markers of IL-6 decreased 80%, and CRP by >50%. Temperature and O2 sats also improved to normal, and suffice it to say, the patient had minimal symptoms! Similar occurrences in the 2nd case study. There is more research underway on this adjunctive use as it relates to acute infections and respiratory infections, which is great news!
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7675307/; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8137825/
Other forms of inflammation that tVNS has been studied for its positive effects are:
- chronic migraines (https://pubmed.ncbi.nlm.nih.gov/26156114/)
- recovery after traumatic brain injury (https://pubmed.ncbi.nlm.nih.gov/25368644/),
- insulin action influencing liver immunologic regeneration, (https://pubmed.ncbi.nlm.nih.gov/26947072/)
- gastrointestinal dysfunction like IBS and chronic pain (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5859128/).
- depression (https://pubmed.ncbi.nlm.nih.gov/25963932/)(we know that many mental conditions like anxiety and depression have an inflammatory component related to the gut).
How do I get better vagal tone?
The tVNS is supposed to be an adjunct to other lifestyle factors that have also been shown to improve HRV. Vagal motor flow, as measured by HRV, has been shown to change with things like:
- Enjoyable aerobic exercise
- Meditation
- breathing practices that emphasize expansive breaths and a longer exhale
- gratitude practice/stopping to “smell the roses”
- humming/singing, and gargling (interestingly enough!)
One could argue that manual therapy practices that make you feel good and relaxed – from acupuncture, to craniosacral therapy to massage – would have a similar stimulating effect on the vagus nerve. So, the answer depends on what sort of input the body is registering from your internal world (the pattern of your thoughts about yourself, other people, life circumstances) and your external world (the type of movement practice/exercise you choose, the type of food you eat, mechanical forces like impact injuries or static posturing).
What the vagus nerve regulates:
- Respiration
- Heart rate
- Gut motility
- Immune system response
Signs your vagus nerve may need additional support:
- You have extreme fatigue from a chronic infection or Covid (long hauler’s syndrome)
- Feel easily overwhelmed/anxious/tend towards depression or have had treatment resistant depression
- Constipation or Irritable bowel syndrome
- Migraines/headaches
Ways to support your vagus nerve:
- Breathing that emphasizes exhale>inhale or breath hold
- Meditation
- Humming, singing, gargling/guttural sounds
- Transcutaneous vagal nerve stimulation
- Body work
- Enjoyable aerobic exercise
tVNS is something I have used personally as well as trialed with a few friends who have all had positive benefits from decreasing nausea, chronic pain levels (75%!), improving bowel movements, energy levels, and the ability to calm the mind. One person felt great for a few days, and then got worse, so this is something that should be consulted about. We have a unit at the clinic that we loan out and they are also easily obtainable for self purchase. If this article piqued your curiosity, consider scheduling an appointment to learn about whether this is something you would benefit from or how to set up this modality for yourself.